Understanding Gastroscopy
Procedure Overview
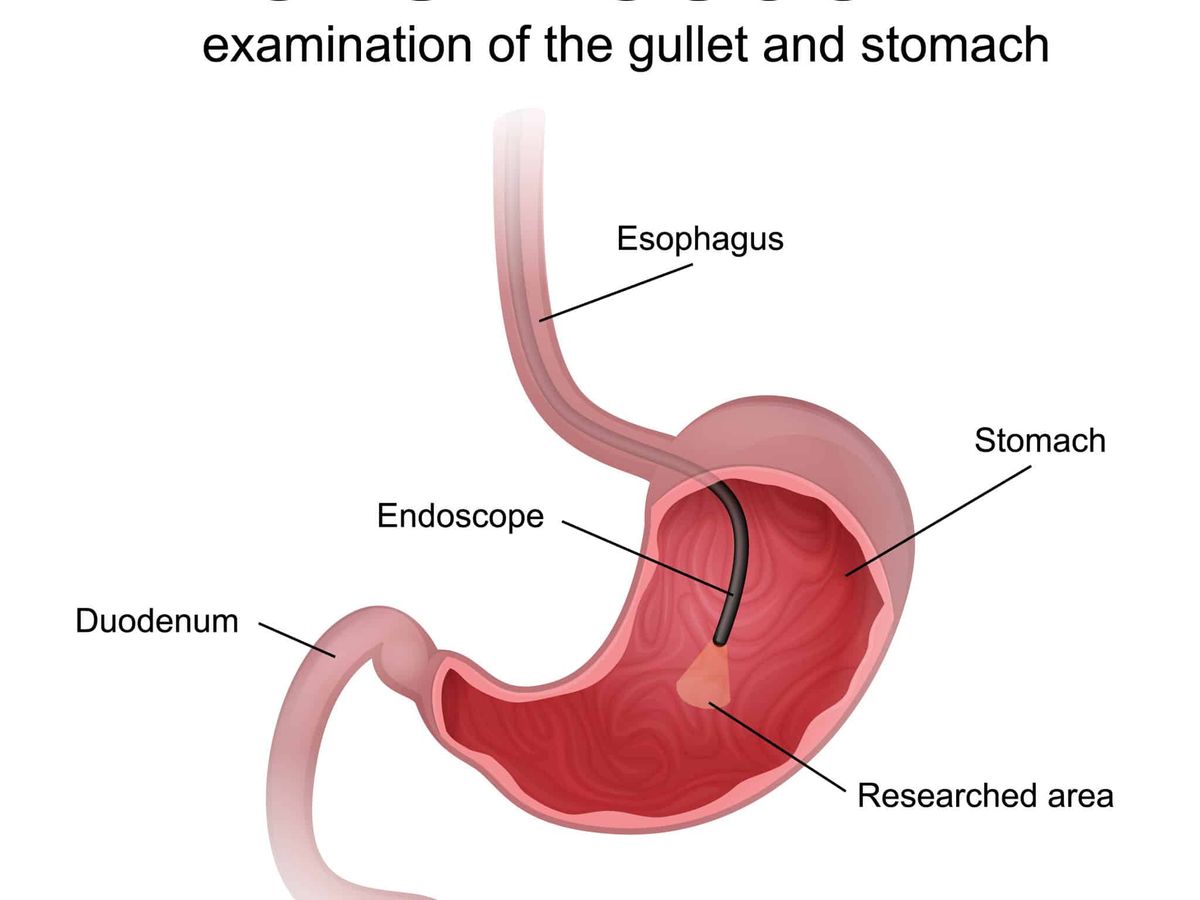
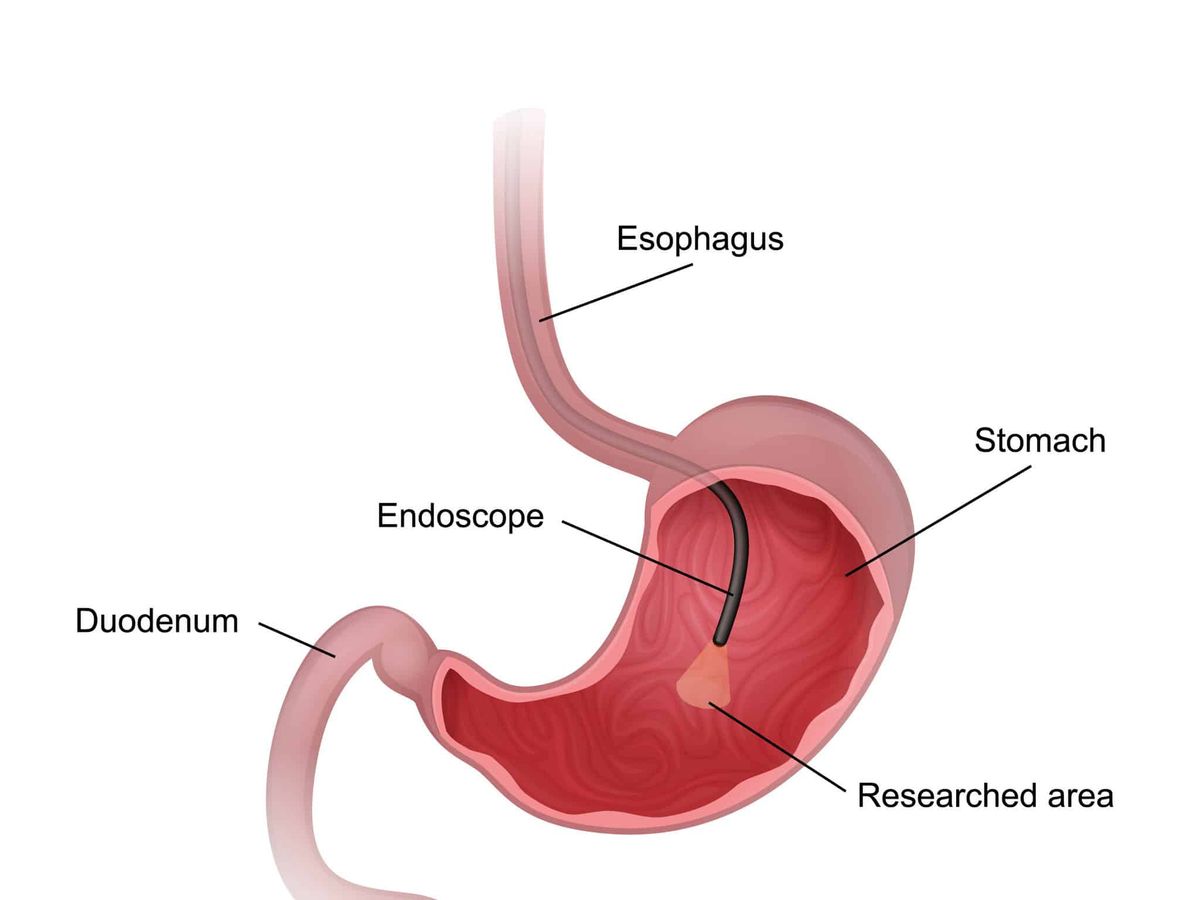
A gastroscopy, also known as an upper gastrointestinal (GI) endoscopy, is a procedure used to examine your oesophagus, stomach, and the duodenum, which is the first part of your small intestine. During the procedure, a gastroenterologist inserts a small tube called a gastroscope into your mouth. This tube, about the size of your pinky finger, has a camera on the end. The doctor gently feeds the gastroscope down your oesophagus to your stomach and duodenum. The procedure usually takes about 10-15 minutes.
Preparation Guidelines
Preparing for a gastroscopy involves several steps to ensure the procedure goes smoothly:
- Fasting: You will need to fast for about 6-8 hours before the procedure. This means no food or drinks, including water.
- Medications: Inform your doctor about any medications you are taking. You may need to stop certain medications before the procedure.
- Consent: You will be asked to sign a consent form to authorise the procedure.
Recovery Process
After the gastroscopy, you will be monitored for a short period to ensure there are no immediate complications. Most people can go home a few hours after the procedure. It’s normal to feel a bit groggy if you were given a sedative. You might also have a sore throat for a day or two.
Gastroscopy is a common and safe procedure, and most people can resume their normal activities within a day.
Choosing a Gastroenterologist
Qualifications and Experience
When selecting a gastroenterologist, it’s crucial to consider their qualifications and experience. Ensure the specialist holds current medical registration and has completed the necessary training. Look for those who have extensive experience in performing gastroscopies and managing gastrointestinal conditions.
Patient Reviews
Reading patient reviews can provide valuable insights into a gastroenterologist’s practice. Look for feedback on their bedside manner, the clarity of their explanations, and overall patient satisfaction. Reviews can often highlight the strengths and weaknesses of a specialist, helping you make an informed decision.
Cost Considerations
Understanding the costs associated with a gastroscopy is essential. Out-of-pocket expenses can vary, so it’s important to discuss fees upfront. Some specialists may offer no-gap services for privately insured patients, which can significantly reduce your expenses. Always check if there are any additional costs for follow-up visits or further treatments.
Choosing the right gastroenterologist can make a significant difference in your healthcare experience. Take the time to research and select a specialist who meets your needs and expectations.
For more information, you can visit Healthdirect.
Gastroscopy Equipment and Technology

Endoscope Types
Gastroscopy relies on a flexible tube called an endoscope. This tube, about the size of a pinky finger, has a camera at its tip. The camera allows doctors to see inside the oesophagus, stomach, and the first part of the small bowel. There are different types of endoscopes, including standard and high-definition models. High-definition endoscopes provide clearer images, which can help in identifying issues more accurately.
Sterilisation Procedures
Sterilisation is crucial in gastroscopy to prevent infections. The endoscopes and other equipment must be thoroughly cleaned and disinfected after each use. This process involves several steps, including pre-cleaning, manual cleaning, and high-level disinfection.
Proper sterilisation is essential to maintain patient safety and prevent the spread of infections.
Image Capture Systems
Modern gastroscopy equipment includes advanced image capture systems. These systems allow doctors to take high-quality images and videos during the procedure. The images can be used for diagnosis and to plan further treatment. Some systems even offer real-time video streaming, which can be useful for teaching and consultations.
Potential Risks and Complications
Infection Control Measures
Gastroscopies are generally very safe, but like all medical procedures, there is always a risk of complications. One of the primary concerns is infection. To minimise this risk, strict sterilisation procedures are followed. Hospitals and clinics ensure that all equipment is thoroughly cleaned and disinfected before each use. Additionally, healthcare providers adhere to stringent hygiene protocols to protect patients.
Anaesthesia Options
Anaesthesia is used to make the gastroscopy procedure more comfortable for patients. There are different types of anaesthesia available, including local anaesthesia, sedation, and general anaesthesia. The choice depends on the patient’s medical history and the complexity of the procedure. It’s important to discuss any previous anaesthetic experiences or allergies with your doctor to ensure the safest option is chosen.
Post-Procedure Monitoring
After the gastroscopy, patients are monitored to ensure there are no immediate complications. Common post-procedure issues include mild throat discomfort and bloating. Serious complications, such as bleeding or bowel perforation, are rare but require immediate attention. Patients are usually advised to rest and avoid strenuous activities for a short period following the procedure.
While gastroscopies are generally safe, it’s crucial to follow all pre- and post-procedure instructions provided by your healthcare provider to minimise risks.
Gastroscopy in Special Populations
Paediatric Considerations
When performing a gastroscopy on children, special care is needed. The equipment used is often smaller, and the procedure is usually done under general anaesthesia to ensure the child remains still and comfortable. Parents should be informed about the process and what to expect. It’s important to choose a facility experienced in paediatric gastroscopy to ensure the best care.
Elderly Patients
For elderly patients, gastroscopy can be more complex due to the presence of other health conditions. Doctors may need to adjust the sedation levels and take extra precautions to monitor the patient’s vital signs throughout the procedure. Recovery might also take longer, and there could be a higher risk of complications. It’s crucial to discuss all potential risks and benefits with the healthcare provider.
Pregnancy Precautions
Gastroscopy during pregnancy is generally avoided unless absolutely necessary. If the procedure is required, it is typically performed in the second trimester to minimise risks to the mother and baby. The use of sedatives and anaesthesia is carefully considered, and non-essential procedures are postponed until after delivery. Always consult with both a gastroenterologist and an obstetrician to ensure the safety of both mother and child.
Always consult with your healthcare provider to understand the specific risks and benefits of gastroscopy in your situation.
Legal Disclaimer: The information provided in this article is for general informational purposes only and is not a substitute for professional medical advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition.

